With contractions 2-3 minutes apart and dilation progressing, I was admitted to the hospital on Sunday, May 25. It was looking like I would deliver that night, but after cortizone shots for Little Q’s lungs and procardia to slow my contractions, I found myself transferred from Labor and Delivery to the Mom Unit about 24 hours after being admitted.
The Mom Unit is where you go if your symptoms are such that it is too risky to send you home on bedrest, but your labor is not so imminent that you have to stay in labor and delivery.
Life on the Mom Unit is not all bad.
It’s tempting to sit here and complain about how hard it is to be hospitalized on bedrest. To have to lie in a hospital bed indefinitely to care for the baby growing inside you, while your 16-month-old daughter is sick and being shuffled (sometimes several times a day) from person to person. It’s tempting to even complain about merely lying still for weeks, when you’re a person who loves action and doing everything yourself. And the mental battles you face with so much time on your hands. And how hard it is to actually rest in the hospital, with a constant stream of high risk specialists, ob residents, nurses, neonatologists, consultants, housekeepers and dietary aides flowing in and out of your room day and night.
But every day you are on the Mom Unit is a day that your baby is not in the NICU. Every day on the Mom Unit buys your baby one more day in the womb, where he can grow and thrive like he was created to.
It means your baby will have stronger lungs, fewer surgeries, fewer long-term physical problems. And for the lucky few, it means delivering a completely normal, full-term baby!
So Life on the Mom Unit is (in retrospect) a very happy thing! I would do it again in a heartbeat.
Of course, while you’re there, it can feel like a trial.
Most mornings I was awakened around 5:30 a.m. when the residents did their rounds. When there was a pelvic exam, it was hard to go back to sleep.
But on the mornings without them, I went back to sleep, and woke again later when the nurses’ shifts changed around 7, and then enjoyed breakfast in bed. On this end of bedrest, I have to say, having breakfast in bed was enjoyable while it lasted!
Everyone complains about hospital food, but I usually enjoy it: fruit, muffins, the expensive yogurt brands, cereal–all foods I like! And they even let me drink coffee, which surprised me a bit. Somehow I thought the hospital wouldn’t serve coffee for a pregnant woman on bedrest with preterm labor!
As always, the reassuring sound of Little Q’s heartbeat was constantly in the background, and in case I wondered if my contractions really were that close, all I had to do was glance over at the monitor. The circulation cuffs always made my legs sweaty, especially overnight.
I frequently slathered Bath & Body Works Sweet Pea Body Cream on my legs because they were dry and itchy. The circulation cuffs heating my well-lotioned legs filled my whole room with the “sweet pea” scent. The housekeeping lady always commented how my room smelled sweet like lotion–and not like a hospital. If I’m gonna be here till week 36, I’m going to do my best to make it an enjoyable experience–for me and everyone else!
When I came to the Mom Unit, they told me I was allowed to get up once a day to shower and get ready, but other than that I could get up only to use the bathroom. I decided to really enjoy the morning routine! My morning shower-and-get-ready routine was the highlight of my day, the only break from the bands on my tummy and my legs. My once-a-day chance to get up and stretch and remember what it was like not to lay in a bed.
I even had time to paint my fingernails and toenails–something I was pretty sure I wouldn’t have time for after the baby came!
During the first week, Daniel came up to visit once. Mara came down with a high fever, which fluctuated between 103 – 105 for about 4 days. We didn’t know (until after her fever broke and she developed a rash) that she had roseola. So Daniel and Mara stayed away from me, not wanting me to catch whatever she had, and risk having a high fever during Little Q’s delivery. Which left me alone in the hospital for days . . . I missed them, my little family!
Every day there was discussion of my leaving. And every day there was discussion of my staying on the Mom Unit until week 34. Depending on who I talked to, I got different answers. And if a nurse happened to adamantly share the “latest” she had heard from “Dr. so-and-so,” it was probably wrong. I was dealing with residents primarily, who would give me their prognosis and recommendations, and then go discuss it with the chief resident. They would further discuss my situation with a panel (including high risk specialists) each morning.
I would have done myself a huge favor if (from the beginning) I had realized the recommendations were completely arbitrary until after they had gone through the whole chain of command. And even then, they were subject to change the next day.
As it was, I would hear the resident say, “We’re going to dismiss you later today after your ultrasound, and you will be on bedrest at home, taking procardia until week 36.” So I would call Daniel to work out who could pick me up, how that affected who was caring for Mara, etc. Once we had worked things out, the chief resident would come in and say, “Change of plans: We’re going to try taking you off the procardia and observe you for 24 hours to see if the contractions continue.”
Daniel and I felt that was a ridiculous idea, since I’d had contractions for weeks before the procardia. The idea was that, sometimes, giving your body a break from the contractions (through use of medicine) and several days of rest may allow you to come off the medicine without contractions. I would have been “game” if my contractions had been fewer, but as it was, the textbooks would tell you I was in active labor the whole time. So reluctantly I went off the procardia.
I didn’t have to wait 24 hours.
Of course, the contractions came back–with a vengeance–so they put me back on procardia and had to watch me another 24 hours to make sure the procardia could actually keep me from dilating more, before releasing me.
It was so frustrating because I talked to different people all the time, and there was not one main person to ask. I felt at the mercy of whoever was on duty that shift, regardless of whether or not they knew anything about me prior to their shift that day.
Finally Thursday afternoon, they decided to let me go home on bedrest, taking procardia until week 36.

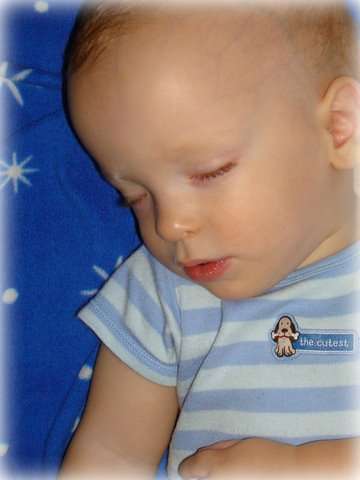
 When Micah was first born, I got him a blue Carter onesie that says, “The Cutest.” Actually, I got two: one in newborn size, the other in 12 months. When he was born premature at 32 weeks, it seemed incredibly encouraging to think past the baby stage and to imagine him as a one-year-old little boy. I think buying a 12-month set of onesies gave me a sense of hope and confidence that there really was an end to all the preemie craziness
When Micah was first born, I got him a blue Carter onesie that says, “The Cutest.” Actually, I got two: one in newborn size, the other in 12 months. When he was born premature at 32 weeks, it seemed incredibly encouraging to think past the baby stage and to imagine him as a one-year-old little boy. I think buying a 12-month set of onesies gave me a sense of hope and confidence that there really was an end to all the preemie craziness